According to a survey conducted in 15 major cities in the U.S., new patients need to wait up to 24 days to get an appointment with a physician. Many of them decide to call the emergency room to avoid delay.
In contrast to this, the famous telemedicine app Doctor On Demand connects patients with a physician through a video call just in 10 minutes and is available 24/7.
The necessity of telemedicine became absolutely evident as we faced the fast-spreading COVID-19 pandemic. Almost overnight, people stopped going out of their homes even to visit a doctor. But staying at home, they still need medical help.
Even though there are many telehealth platforms in the circuit, loads have increased and new apps are in demand.
In this article, we’ll try to answer the question of how to start a telehealth business. Read on!
What is Telemedicine?
Telemedicine is a term used to describe remote clinical services like diagnostics and monitoring. Often, telemedicine is used as a synonym of telehealth, but according to the United States Department of Health and Human Services telehealth is a broader term that also includes administrative meetings and continuing medical education.
Telemedicine began with the invention of the telegraph. Then the appearance of telephones brought medical assistance to remote areas. The Red Cross and other health organizations could use the phone in hot spots.
In our days, telemedicine has broadened its implementation scope and has become available on-demand for everyone. Why is it important to continue investing in telemedicine app development and how can it change our attitude toward medicine in the next few years?
Benefits of Telemedicine for Patients and Physicians
The traditional clinical approach is incomplete without the possibility to provide help remotely to those who cannot reach the hospital. With telemedicine, it has become possible to close this gap, and has given many benefits to both doctors and patients:
1. Mitigating the risks of visiting contagious patients. Telehealth allows doctors to stay safe while avoiding face-to-face interactions with sick patients. This advantage became much more evident during the COVID-19 pandemic. Telehealth apps allow medical staff to continue serving patients online, without the risk of getting sick. As a result, such online diagnostics and monitoring can help flatten the curve in times of a major health crisis.
“For clinicians who are self-isolating or under quarantine, video consultation allows them to continue treating patients. In such crucial times, we know that every doctor available to help the situation counts. Beyond COVID-19-specific consultation, we also need these doctors to continue providing primary care – through telehealth – for ailments like eye infections, skin conditions, urinary tract infections, and chronic diseases, etc.,” — said Dr. Kevin Kok, a practicing doctor and chief operating officer of Doctor Anywhere.
2. Availability of specialists. Many people living in small cities or remote areas cannot easily reach the necessary specialists. In the USA, there is an average of 40 doctors available for every 100,000 patients living in rural areas. Due to telemedicine, doctors are available despite the distance. Patients do not need to make long trips to a healthcare facility when it’s not obligatory. It is essential for the disabled, elderly people, and kids, who cannot easily travel.
3. Time-saving. Most hospital visits are basic and can be handled easily via a phone or a video call. When you need to refill your prescription, it can be really frustrating to go to the doctor’s office, waste time in traffic, and wait in line. Instead of this, having a video conference with a doctor can quickly and effortlessly answer patients’ questions and save hours.
4. Less medical staff burnout. The biggest part of a physician’s day is spent on red tape like collecting the patient’s history, entering data into the patient’s profile in the EMR, and making reports at the end of the day. A telemedicine app can automate most of these tasks. giving doctors an opportunity to better schedule their days and feel better.
5. Cost-effectiveness. As most of the administrative duties are handled by the app automatically, doctors can spend more time with patients. As a result, their client load expands, and profits increase.
6. Preventing patients’ data loss. Cloud-based telemedicine platforms are able to collect, process, and securely store huge amounts of information. The data entered into the app can be synchronized with electronic health records (EHR) used by the patient’s regular doctor. This allows doctors to easily access each patients’ health history and have a 360°-view of their health status, previous diseases, and prescriptions. This will allow them to make more accurate diagnoses.
Why Start a Telemedicine Business App Today?
Not only doctors and patients can benefit from the advantages of telemedicine. Entrepreneurs who start a telehealth business now will be profitable for many years to come.
For example, one of the most popular telemedicine applications is Doctor-on-Demand. They serve 1 million registered users. More than 80% of their appointments are repeat visits. In 2019, they had more than 2 million video-visits and their revenue was $12 million. But can a new company have the same success?
Before we drill down into the question of how to start a telemedicine practice, we should answer the question, WHY?
Here some of the most obvious reasons why telemedicine is going to become widespread in the next decades:
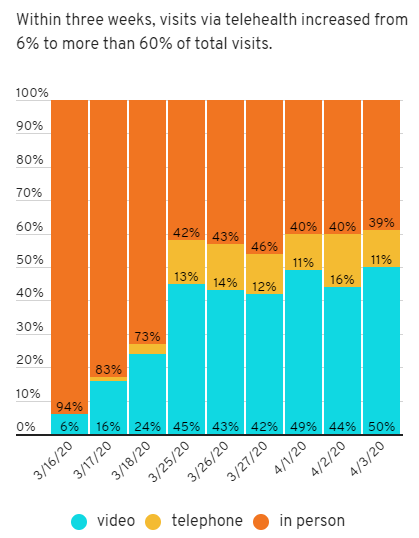
1. An extreme surge in the demand for telemedicine apps and an increase in revenues.
The global telemedicine market is projected to reach $185.66 billion by 2026. To compare, in 2018, it was $34.28 billion.
The COVID-19 outbreak in 2020 has triggered the use of remote diagnostics and monitoring due to its extreme ease of transmission, the shortage of medical specialists, and too few hospital beds.
Physicians, who only work offline in clinics or have a private practice were forced to look for online platforms to continue their work. Otherwise, they would have had to halt their practices.
UC San Diego Health reported that half of all outpatient visits in recent weeks were through video. Luckily, the medical center had already established a telemedicine system in place several years before the COVID-19 pandemic.
2. Fewer legal limitations.
In connection with COVID-19, many federal telemedicine regulations were eased or removed completely. Telemedicine was recognized as an indispensable tool for the prevention of the coronavirus spread.
According to the latest legislation, the Department of Health and Human Services’ Office for Civil Rights (OCR) allowed public messengers like Skype, FaceTime, Facebook Messenger, Google Hangouts, and Zoom to be used for telemedicine services, disregarding possible risks of personal data disclosure. The government will not impose penalties on the medical platforms that do not comply with HIPAA rules during the COVID-19 emergency.
Disclaimer! In different countries and even states the laws can vary, so follow your area regulations when you start the development of telemedicine apps.
Post-quarantine, the role of telehealth, and its benefits will definitely be reevaluated and new simpler regulations for telemedicine startups. Moreover, Medicare and other health insurance programs already cover some or all telemedicine services.
3. Increase in the elderly population.
The number of people over 65 is growing rapidly, as well as the number of nursing homes and assisted living facilities. Telemedicine is indispensable for these facilities. Individual caregivers need to have access to immediate medical consultation for patients who cannot be easily transferred to the hospitals. It was estimated that using telehealth in nursing homes could prevent 387,000 unnecessary hospitalizations, saving up to $327 million each year.
Moreover, many elderly people prefer to live at home, but they still need remote monitoring and online consultations.
4. Streamlined IoT technologies adoption.
Each year more and more smart devices and new technology enter the field of Healthcare:
a. Using wearables allows the monitoring of blood pressure, temperature, pulse, sugar level, and total activity rates. These IoT devices can transmit data to the telemedicine apps, and physicians can remotely monitor the health of their patients who stay home. DictumHealth created a virtual solution that tests the patient's vital signs, with the accuracy of hospital exams, remotely. For instance, such tests can be performed far from the hospital, even in very severe conditions, like onboard a ship in the middle of the ocean. Then the data is sent to the physician for a diagnosis.

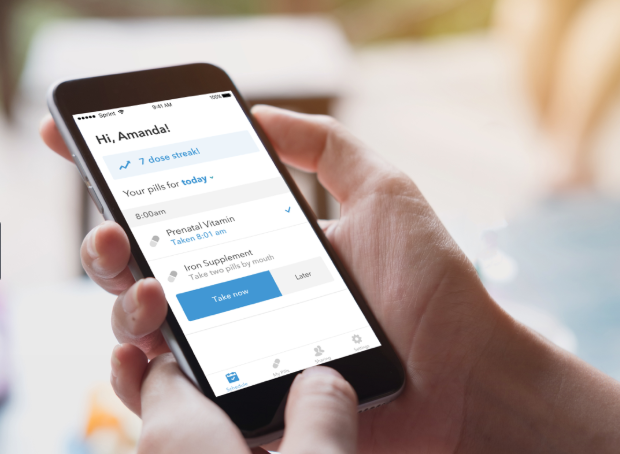
b. Another advantage of telemedicine apps is their integration with pharmacies to seamlessly order and ship medicine to patients. IoT technologies introduce devices like Pillsy, a smart medication bottle that connects to an app. This gadget not only reminds people to take their medicine, but also measures the exact dose each time the patient opens the bottle, notifies the relatives if the patient didn’t take the pills as prescribed, and e-mails pharmacies to re-order the medications.
c. Some patients need strict monitoring when taking medicine. For example, people with mental disorders. It is now possible to make pills with sensors inside that interact with patches worn on the body and allow the app to track if the patient took the pill or not.
All of these and many other new technologies that are coming in the nearest future will open unlimited opportunities for telemedicine development.
Challenges of Telemedicine Business
Besides all the obvious benefits of telemedicine, there are still many hurdles in the way of telemedicine startup development and adoption by the public. Here are some of the most common:
- Scalability
While creating a telemedicine app, founders should anticipate sudden spikes of user activity. The outbreaks of epidemics can occur without notice, as did COVID-19. You should be sure that your app is scalable and will not fail under heavy traffic.
- Security
Patient personal data is highly sensitive and its protection should be your top priority. Unfortunately, cyber-attacks at hospitals have become more frequent.
One of the most recent cases happened in the Czech Republic during the outbreak of the coronavirus pandemic. Brno University Hospital’s information system was hacked causing all computers to shut down. This prevented data from being transferred among the laboratories and all other departments. The hospital staff had to write and transfer notes manually, which slowed all the processes and endangered patients’ lives.
To protect your system, you should implement multi-step authentication using biometric identification (face or fingerprint recognition), data encryption, backup, and recovery procedures.
- Healthcare legislation
Depending on the country, the laws pertaining to data collection, storage, processing, and sharing may be subject to different regulations and laws. Learn about HIPAA if you build your app for the US market, PIPEDA — for Canada, or Data Protection Directive 1995/46/EC and the e-Privacy Directive 2002/58/EC for the European Union.
To protect your customers’ data and avoid huge penalties from the auditing authorities, those who are going to build telemedicine platforms should choose a development company that will create a system that complies with regulations.
- Insurance services
Until it gains equal status with traditional medicine, Medicaid and other insurance companies are not eager to reimburse bills from telemedicine. Thus, many people hesitate to use telehealth apps, as they will need to pay for online medical visits out of pocket.
Technological progress can streamline the adoption of telemedicine services by Medicaid and other insurances. In 2017, Medicaid provided reimbursement for remote patient monitoring in 22 states. The pandemic situation of 2020 has forced Medicare and Medicaid to expand telehealth coverage to provide virtual diagnostics and monitoring to more patients.
- Patients' trust and doctors' validation
One more challenge for the platform’s owners is to gain the trust of their customers. Patients want to be sure they are served by experienced doctors whose reputation is verified. The platform Admins should validate all the doctors who register on the platform before giving them access to the patients’ appointments. Later on, we’ll show how this is done.
- Technological barriers
Telemedicine works only through the Internet. Moreover, broadband should be powerful enough to allow video-conferencing. This can be a challenge for many areas and households.
Over 40 percent of Americans with an income of less than $30,000 a year don’t have Internet at home, 46 percent don't have a computer and 29 percent do not use a smartphone. Unfortunately, in rural areas, the Internet is still poor, which presents obstacles to telemedicine adoption.
Another problem is technology adoption by elderly people. Only 26% of seniors feel confident using smartphones, computers, and other devices for their needs due to technical, physical, and memory challenges. It is important to make the website usable for people with disabilities. Pay attention to web accessibility principles to address this challenge.
Don’t ever leave the patients alone with the platform. It is important to provide the support of a human specialist. Combine technology with human assistance. For instance, SWORD Health, a health-tech company providing a platform for physical therapy at home, uses a combination of AI and human specialists. A physiotherapist monitors the patient's performance to make changes to the treatment plan and communicate with the patient.
Need an estimation of your telemedicine app development?
Contact UsTypes of Telemedicine and Areas of Implementation
If you want to get a clear picture of how to set up a telemedicine center, you should be aware of different types of telemedicine and their purpose. Telemedicine is subdivided into different types by application, by modality, by the end-user, and by purpose. Let’s review this terminology.
1. By Application
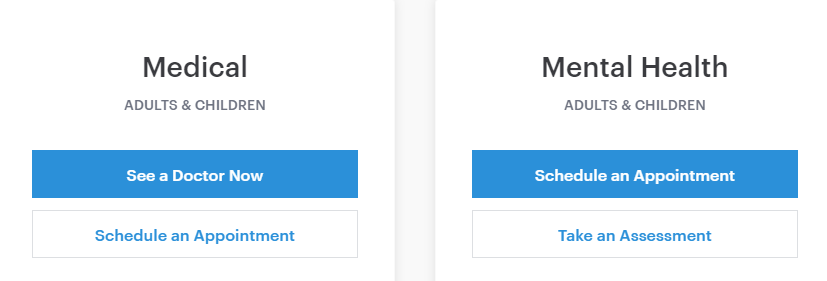
There are many areas of medicine where telemedicine evolves quicker than in others. The most popular now are teleradiology (analysis of radiology images), teledermatology (diagnostics of skin problems by photo), telepsychiatry (online sessions), and telecardiology (examination of ECG images).
2. By Modality
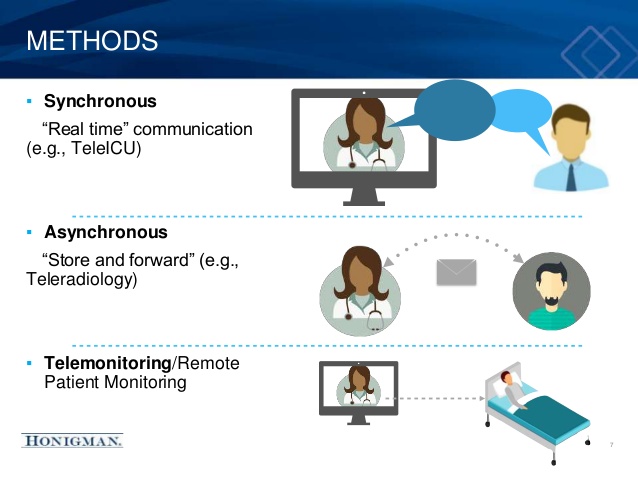
Here we can divide telemedicine into real-time (synchronous), store-and-forward (asynchronous), and remote monitoring.
- Synchronous, or real-time, means interactive audio or video consultations between a patient and doctor that require the online presence of both at the same time. This type relates to apps that focus on emergency situations. Real-time consultations allow a more complete understanding of the patient’s problem during the online examination.
- Asynchronous is used when the app first collects medical history, images, and pathology reports; and then transmits this data to the physician for assessment when convenient. This is used in non-emergency situations. The patient has no need to wait for a doctor in real-time when there is no urgency. Such waiting can be unacceptable when there is a high load or shortage of specialists.
- Remote monitoring refers to continuous tracking of a patient’s health through video monitoring, lab tests, images, or data from wearables provided by the patient. This is ideal for long-term monitoring of chronic diseases or conditions of elderly people. For example, GlobalMed provides a variety of remote monitoring solutions and devices.
A telemedicine app can specialize in one, or a combination of these types. The choice of modality will influence the scope of necessary features.
3. By the End-user
Telemedicine apps can be focused on either medical facilities or homecare.
Telemedicine is already actively used by hospitals for distant surgery and consultations, and for pre-hospital care in the ambulance. It is used in assisted living facilities and nursing homes.
The home care segment has only started to grow in recent years and is anticipated to revamp the traditional way patients get care. Its use will accelerate as telemedicine becomes more available and affordable.
4. By Purpose
The main reasons why people use telemedicine software are as follow:
- Medical consultation. In many cases, people do not need a doctor examining them in-person. Using a chat or video-call, it's easy to describe the symptoms of flu or infection, to share photos of the skin for some dermatological issue, or to send the already collected analysis results. The online doctor can make a diagnosis using the information to prescribe treatment and medications or to refer the patient to a specialist for further examination.
- Prescription renewals. Prescription refilling is a constant concern for people who need particular medicines for extended periods. Telemedicine can remove the necessity to visit a doctor each time they renew their prescription.
- Access to medical records. When they visit different medical specialists, people may need to tell them about their previous medical history and their history of treatment. It can be difficult to remember everything, and papers can sometimes be lost. So, having a telemedicine app that stores the patient's history is beneficial for tracking health history throughout life.
- Support for EMS. Telemedicine can help in areas experiencing a lack of Emergency Medical Services (EMS) specialists. The telemedicine functionalities for EMS include real-time audio and video communication, instant image transmission, and a 12-lead electrocardiogram. Thus, hospital specialists can provide their expertise and diagnose patients remotely, in the ambulance, before they are hospitalized to save precious time.
Telehealth Business Model
When they are wondering how to start a telemedicine business, many people want to know how it can make a profit.
Telemedicine apps usually play the role of a mediator between a patient and a physician. For their services, doctors get paid the same way as in any private clinic. A platform can take its share for the services either from the patients or from the doctors.
A telemedicine app can choose one, or a combination, of the following monetization models:
- Commission. The app takes some percentage of the price for the consultation. It can be a fixed price or rate per minute. The Doctor-on-Demand app uses a fixed fee charging a patient a 25% surcharge on top of the cost of each online appointment, while the Tele Doctoral platform charges $0.08 per minute. The rates can vary depending on the consultation duration, frequency, specifics, or the doctor’s specialization.
- Membership. If your platform is focused on users who need regular monitoring, you can propose monthly or yearly payments. For example, HealthTap takes $119/year for unlimited consultations.
- Software as a service. Instead of providing medical services by yourselves, create software that clinics can use by subscription. For example, Doctor-on-Demand SaaS takes $1 per employee per month.
Competitive Landscape
Telemedicine garners great attention, not only in the US but in many other countries. Let’s take a look at the top telemedicine companies around the world.
| Region | Telemedicine Apps |
| Global | Babylon |
| USA | Amwell Doctor-on-Demand Teladoc Health Global Med Dictum Health InTouch Technologies Inc Snap MD Medici MD live HealthTap |
| Canada | Maple Livecare GOeVisit OnCall Health Akira |
| Europe | Min Doktor (Sweden) KRY (Sweden) Doctolib (France) Push Doctor (UK) OpenTeleHealth (Denmark) Matellio (UK) ZoomDoc (UK) Medgate (Switzerland) Barmer (Germany) OnlineDoctor (Russia) Doctor Smart (Russia) |
| Asia | Doctor Anywhere (Singapore) Halodoc (Indonesia) Speedoc (Singapore, Malaysia) Medihere (South Korea) Hello Doctor (India, Bangladesh, Thailand, Malaysia) Doctor raksa (Thailand) Mfine (India) |
| Middle East | TruDoc 24x7 Health at Hand Cura Okadoc |
| Australia | Doctors on Demand HealthNow Instant Consult |
| Africa | Bisa Tremendoc |
How to Develop a Telemedicine App for Homecare?
The aim of a telemedicine platform is to connect a patient to a doctor through the Internet.
Platforms can function differently. One way is a marketplace where doctors can register by themselves and start providing their services through the online platform independently. Another way is buying or creating software for clinics.
Some platforms allow patients just to connect to the first available doctor to get urgent help. Other platforms allow patients to schedule an appointment with a doctor who has a certain specialization, and some allow patients to choose a doctor based on reviews and profiles. The third type of platform allows for a combination of the two.
Usually, the user workflow looks like this:
- The patient requests a consultation with a specialist and pays the fee online.
- If it's not an urgent call, the patient describes their symptoms (either in a questionnaire or in a text field) and adds photos and lab tests. If the patient needs to have an online consultation immediately, the patient is put in a queue in a virtual 'waiting room’ until a doctor is available.
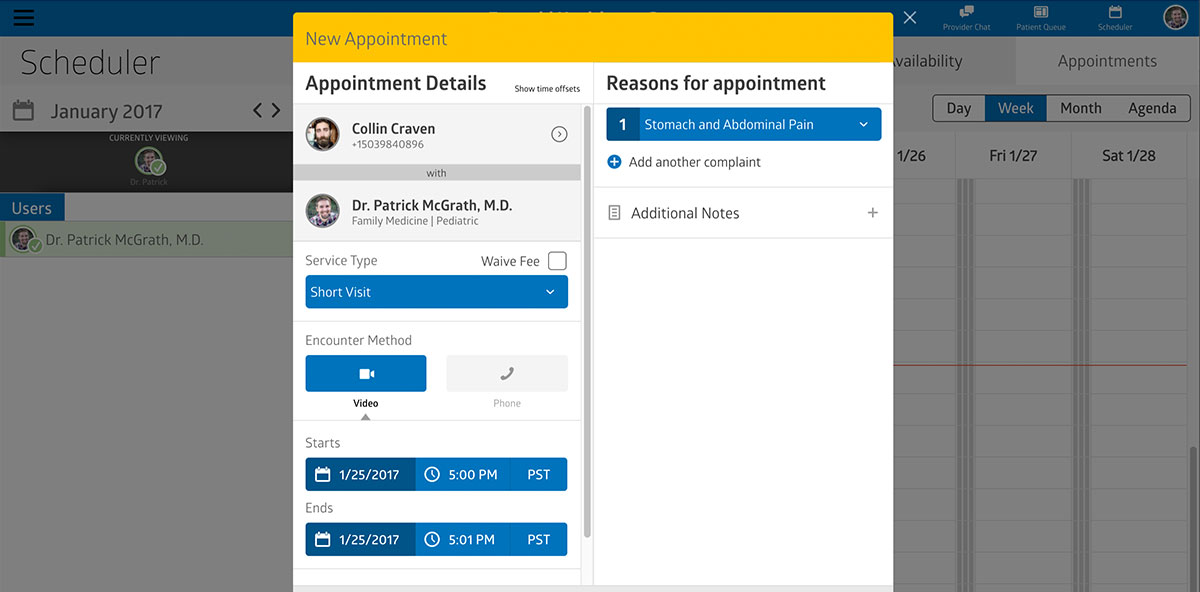
- The doctor confirms the appointment and can view the patient’s profile before the visit.
- During a video-conference with a doctor, a patient shares symptoms, photos, and lab tests. The doctor can ask clarifying questions to make a diagnosis, prescribe treatment, or request an additional examination.
- After a session, the patient can write a review of the doctor and order a repeat appointment if necessary.
- The doctor receives the payment for the consultation.
To build an app for telemedicine, you should consider the following functionalities.
Core Telemedicine App Features
Patient section
Patients should easily be able to book an online visit to a doctor and have a consultation. The following features are needed:
- Registration
Patients should be able to register on the platform by email, mobile phone, or insurance number. The system may ask for the patient’s zip code or automatically identify the geolocation by IP address to match patients to doctors from the same area.
- Patient profile
The patient profile should store the patient's personal data, all appointments, billing information, treatment history, lab tests, and prescriptions.
To save physicians time, patients may be asked to add their health history to their profile. The patients’ data may consist of general personal information, lab test results, photos, MRT, CT, ECG results, and data from digital devices.
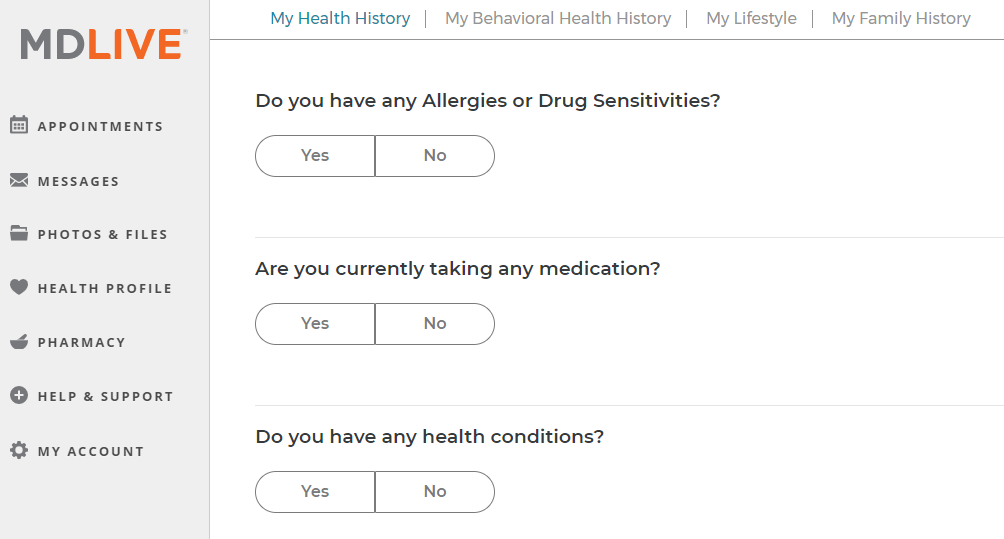
You can include the ability to add external doctors who monitor the patient on a regular basis to seamlessly share medical records. This allows synchronizing the health data for better care in the future.
- Search
If the platform provides a variety of specialists, the patient should be able to search for a doctor by specialization, location, availability, spoken language, and rating.
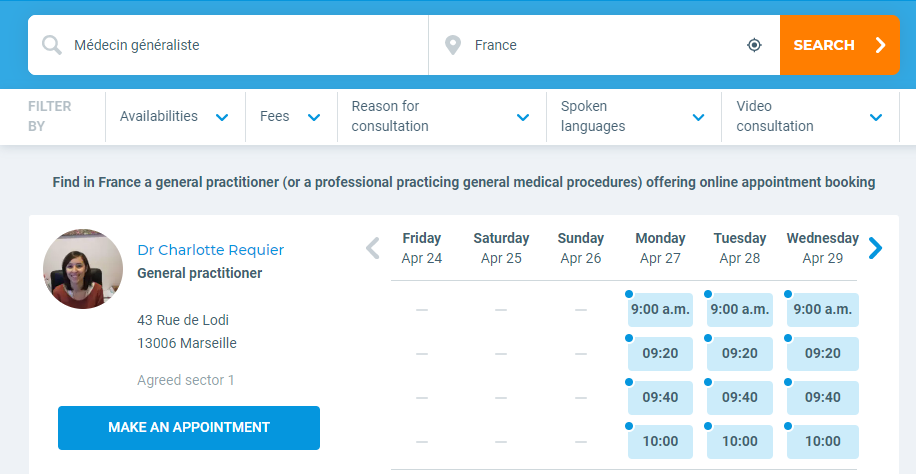
- Appointments
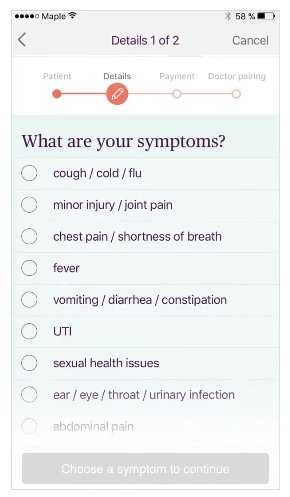
Having found a specialist, the patient needs to be able to check the doctor’s availability and schedule an appointment. In addition, they should have the ability to edit or cancel previously scheduled appointments. Before scheduling an appointment the patient may be asked about her symptoms to identify the urgency of the situation or to help the doctor better prepare for the e-visit.
- Notifications
When the doctor sees the patient's appointment and confirms it, the patient should receive a notification. Other notifications may be used to remind of the time of the appointment or to refill prescriptions.
- Communication
Audio or video-conferencing is an essential part of the online visit. The platforms should provide secure messaging and file transmission. The calls must be saved so that doctors and patients can review them in the future.

- Billing and online payments
Provide the most common and convenient payment methods in your area, and keep a record of each payment in the patient’s Billing History.
- Rating and review
After a consultation, ask users to give feedback on their experience as a whole, and a review of the doctor so other patients can make their decisions more confidently. This is a trust-generation feature that allows you to attract new patients and to encourage the physicians to provide quality service.
In Doctor On Demand, when a patient gives a high rating to a doctor, the system automatically adds this specialist to the patient’s favorites list. The next time the patient needs a consultation, she will see if any of her favorite doctors are currently online and will be able to schedule a visit with them directly.
Doctor section
User-doctors should be able to register and manage their appointments and earnings.
- Registration and verification
Doctors who want to use the system should go through a verification process providing detailed information about themselves and upload their licenses.
A background check for medical licensure, education, work history, and malpractice history can be made through the National Physician Data Base (NPDB) and the American Medical Association (AMA).
- Doctor profile
Physicians should add information about their specialization, education, diploma, license, and experience.
- Appointments
The practitioners should be able to set their availability hours and see all bookings for consultations. They can either confirm or cancel the appointments or propose another time in case of changes in their schedule.
- Communication
This feature is similar to the patient’s communication feature. You can expand it to give the doctor the ability to add notes during the session or to share their screen and show the patient additional, relevant information.
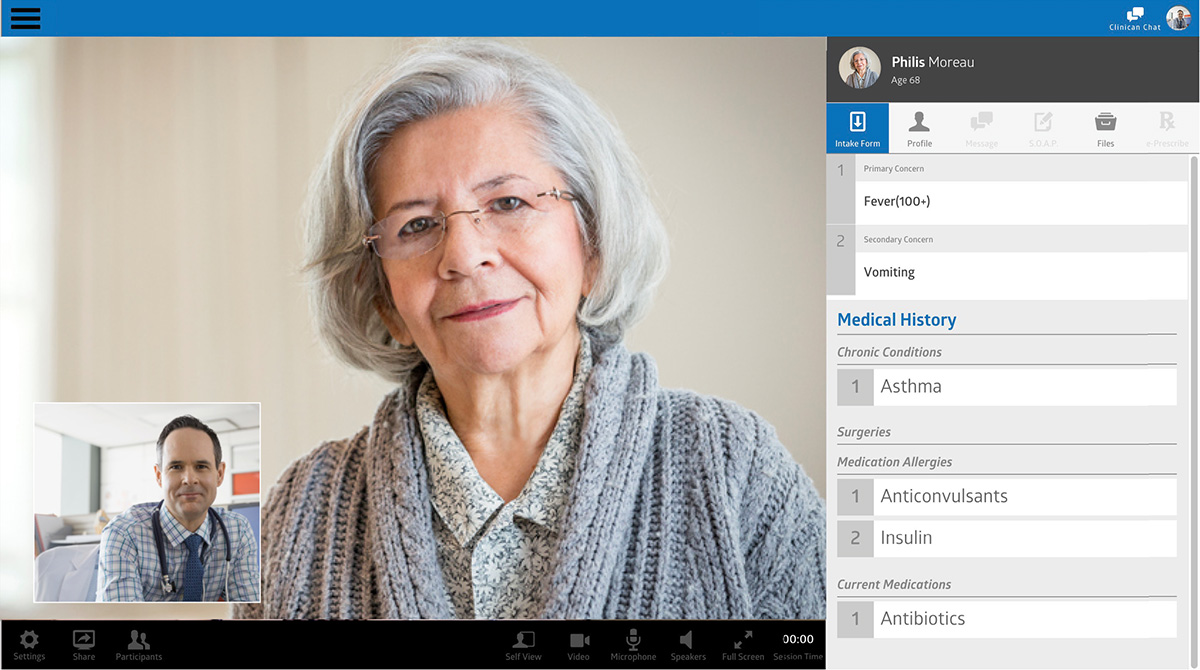
- EMR/EHR integration
All patient information should be transferred to a single EMR or EHR so that any other specialists who work with the patient will be able to check medical history records. In addition, doctors can invite patients directly from their clinics’ EHR to the platform and provide e-consultations.
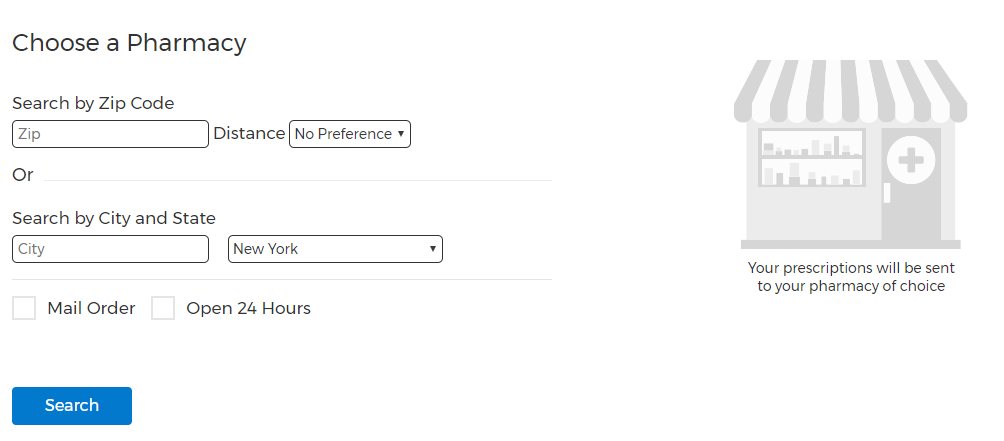
- E-prescribing
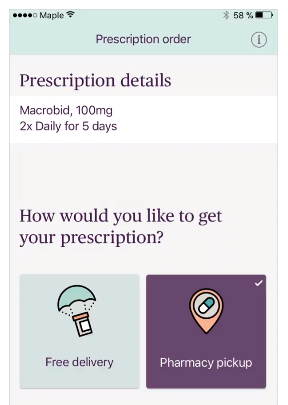
Doctors should be able to write prescriptions and send them out to each patient digitally. Then, the patient will be able to get the medication from a drugstore or order online delivery. Some platforms are integrated with pharmacies or delivery rapid and convenient.
Telehealth providers are not allowed by law to prescribe controlled substances, for example, Xanax. This information must be explained clearly to both patients and doctors in the platform rules. These regulations can be found in the Ryan Haight Online Pharmacy Consumer Protection Act and all telemedicine e-prescriptions are controlled by the Drug Enforcement Agency (DEA).
Some medications can be prescribed or refilled automatically. In order to take advantage of this service, patients must answer questions, or in some cases talk to a doctor.

Doctor-On-Demand - Online prescription
- Earnings management
The practitioners would like to see how much they earn for their consultations. The platform must maintain complete and actuate records of all financial transactions.
Admin Section
This is the back-office of the platform where managers and admins can view the user interactions, generate reports, and manage the website content. It may include:
- Doctor management
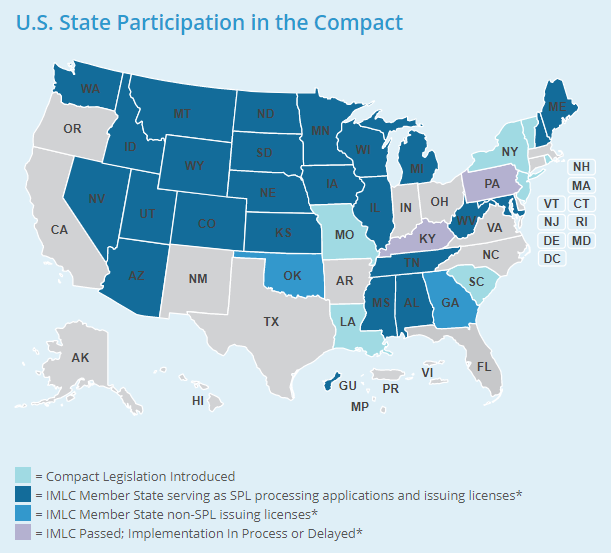
A database of all registered doctors. Each doctor should be verified and either approved or rejected depending on her qualification and license. The physician should be located in the states where they are licensed.
In the US, doctors are licensed to provide treatment in a certain state and cannot provide services in the other states. This means that you need to attract doctors from as many states as possible. Alternatively, you may hire doctors who have several licenses or have been licensed by Interstate Medical Licensure Compact that allows practitioners to work in 24 states.
- Patient management
This is a database of all registered patients and their contacts. In case of a problem, an Admin should be able to log in as a user and make corrections.
- Dashboard
The dashboard is the main screen that displays the overall statistics on performance, users, appointments, finances, and tasks.
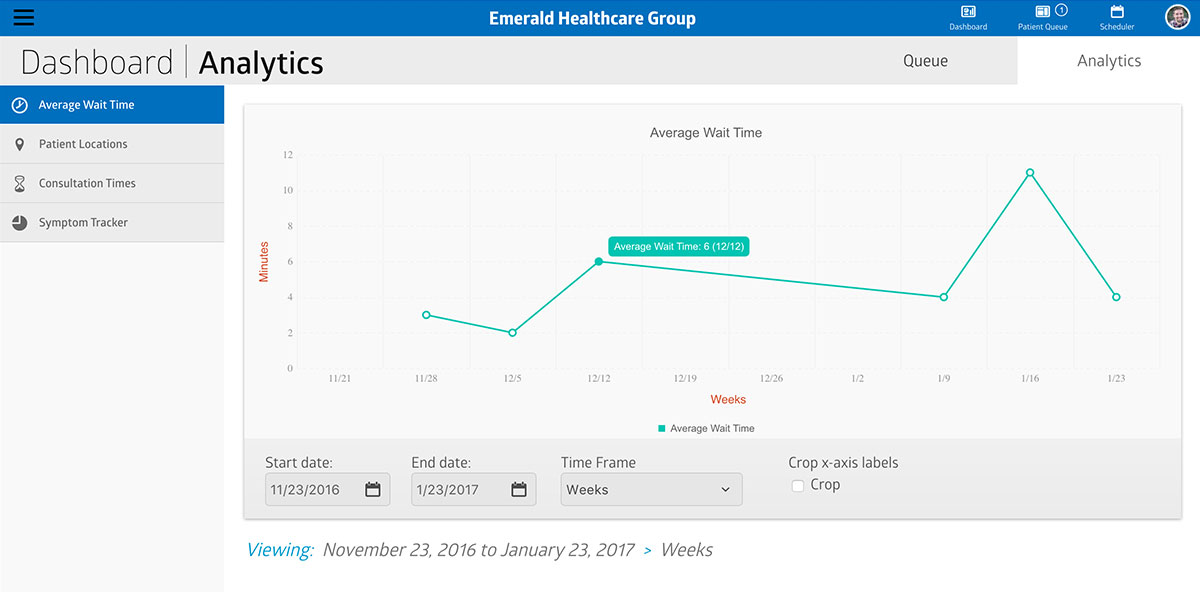
- Reports
Automated reports allow you to quickly view the analytics on different metrics of platform performance, finances, and user actions during a certain period of time.
- Finance management
All transactions through the platform and fees for platform services.
- Learning management
One of the requirements for doctors may be training to get acquainted with the platform and the legalities of telemedicine before they begin seeing patients. Admin should be able to upload and edit courses as well as assign them to providers and track their progress of completion.
- Customer management
All efforts to attract patients, and retain customers should be recorded in the customer relationship management system. An Admin should be able to view the income from each customer, assess their membership type and discounts, and categorize them into groups for future marketing and sales activities.
- Insurance management
This is the system that allows tracking reimbursement from insurance companies.
- Content management
Creating questionnaires and surveys, posting to the blog, and modifying other website content.
- Support
Users may need technical support setting up and managing their accounts and resolving financial issues and conflicts.
Extra Telemedicine App Features
The features listed above are quite standard for any telemedicine application. The below will make your product stand out among competitors.
- AI features
In a telemedicine app, AI features can enhance the user experience and efficiency of medical consultations. For instance, AI-driven medical chatbots can provide initial symptom assessments, directing patients to the appropriate care based on their inputs. Additionally, machine learning algorithms can analyze medical data to predict patient outcomes, personalize treatment plans, or even detect anomalies in patient records and imaging studies, facilitating early diagnosis and treatment adjustments.
To decrease the load on the doctor’s schedule, you can add pre-visit questionnaires for patients that ask them to assess their own health. The patients can be requested to describe their symptoms and to upload photos and lab tests. Some telehealth apps use AI to collect and analyze symptoms and check the database to suggest a possible diagnosis and treatment plan before the patient even sees a doctor.
For example, with the heavy traffic on telemedicine apps due to the coronavirus pandemic, the platforms implemented free COVID-19 risk assessment questionnaires to help people measure the seriousness of their problem.
- Medication tracking
This feature will remind a patient to take necessary medications and to buy the refills in advance.
- Patient insurance plan
This feature can automatically identify what services are covered by the patient's insurance providers. For example, Doctor On Demand is integrated with PokitDok through the API to get information about the services covered by more than 700 insurance providers that cover 93% of the US population.
- Pharmacy databases
Integrate the app with the pharmacy to provide patients and doctors with seamless prescriptions. Users can use the map to find pharmacies nearby.
- Business account
Many companies have already realized the benefits of telemedicine for corporate needs. Instead of asking for a day off to visit a doctor, employees can use a doctor-on-demand consultation. The bill, and sick leave recommendations, will be sent to the company. The Doctor On Demand app is already used by more than 400 employers to provide medical services to their employees.
Telemedicine App Development Cost
The cost of developing a telemedicine app can vary significantly based on the development approach selected.
For entrepreneurs who are mindful of their budget, off-the-shelf solutions can be a practical choice, with costs starting around $5,000 for a basic app or website. However, expenses can increase if there's a need for specialized themes, plugins, and integrations to enhance functionality.
White-label solutions offer a middle ground, leveraging pre-existing scripts that streamline the launch process and optimize costs, with prices ranging from $5,000 to $15,000 depending on the level of customization and additional functionalities required.
For maximum customization and control, custom solutions are the optimal route. Starting costs for a Minimum Viable Product at Greenice begin at $10,000 and can escalate considerably, driven by the complexity of the desired features and the development team’s hourly rates, which vary depending on their expertise and geographic location.
Entrepreneurs must carefully consider the trade-offs between cost, quality, and functionality to select a development path that aligns with their financial constraints and business goals.
How to Apply This to Your Business
Telemedicine was lagging behind traditional medicine for many years because of restrictive laws and fears of competition from traditional clinics.
Only a precedent such as the COVID-19 pandemic exposed the real necessity for digital medical help. The market will grow exponentially as the government eases restrictions for providing telehealth services. Furthermore, in spite of the presence of mighty companies in the market, there is still a shortage of doctor-on-demand solutions.
If you are planning to start a telemedicine app and are waiting for the sign, here it is! Use our article to complete your plan with any missing elements and cast your doubts aside.
Before requesting an estimate of the doctor-on-demand app cost, try to list and prioritize the features you need so that the vendor will be able to give you a more accurate approximation.
The cost of implementing a telemedicine app will depend on many factors: the vendor rates, the complexity of the solution, and changes in requirements during the development process.
The telemedicine startup costs can be reduced if you start with the core features — minimum viable product (MVP) — the basic features that will fulfill the main application purpose. In the future, as the app shows its profitability, you can scale it up, adding more features and enhancing the existing ones.
Send us your request for an estimation today!
Get a Free QuoteRate this article!
5
 PHP Development
PHP Development Laravel
Laravel Yii
Yii






Comments (0)